Blood Group Problems
Problem
Blood group complications can always arise when mother and fetus have different blood groups.
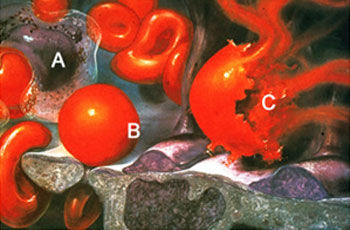
The most common complications of this type are associated with the Rhesus blood group. Where the mother is Rh-negative (i.e. does not have the Rh antigen) but the fetus is Rh-positive, the mother will produce antibodies against the fetal red blood cells if fetal blood enters her bloodstream either during pregnancy or at birth. These antibodies are then carried across the placenta to the fetus, where they burst the fetal red blood cells (illustration). As a result, the fetus becomes anemic and in rare cases may die while still in the mother’s abdomen.
Diagnosis
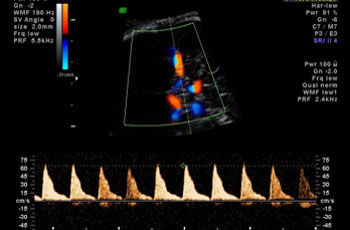
Where anti-Rh antibodies are found in the mother’s blood, the first step is to determine whether the fetus is in fact Rh-positive. The fetal blood group can nowadays be determined directly from the mother’s blood by special molecular biology techniques. Once the fetal blood group has been determined beyond doubt, tests are performed at regular intervals to determine whether maternal antibodies have made the fetus anemic. In this regard our Center helped to develop an ultrasound method which uses blood flow velocity as a marker of fetal blood content. The illustration shows blood flow velocity being measured in a brain artery.
Therapy
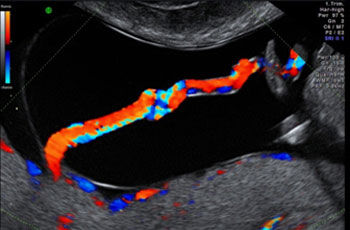
A fetus found to have too little blood requires regular blood transfusions during the pregnancy. These are given by injecting blood directly into the fetal umbilical cord. Special color ultrasound techniques are used to help locate the umbilical cord within the amniotic fluid (1). As the umbilical vein is only a few millimeters thick, the task of inserting the needle calls for an extremely steady hand. Once the tip of the needle has been correctly positioned (2 Video): as indicated by the bright white spot), a small sample of fetal blood is taken to determine the severity of the anemia. The blood transfusion is then administered directly into the umbilical vein. A fast-growing fetus needs transfusions about every two weeks until birth.
Outcome
Over the past ten years we have saved the lives of many children in this way (illustration). The Zurich Center for Fetal Diagnosis and Therapy has far more experience in this field than any other center in Switzerland.